While endometriosis is one of the most prevalent health conditions for women, impacting up to 10% of women globally, it is also surprisingly and tragically misunderstood. In fact, on average, women in the US will suffer from endometriosis for 10 years before a proper diagnosis (1).
Why is there such a massive diagnosis delay if so many women are suffering? To understand this issue and push for a solution, it is necessary to first understand what in the world is endometriosis!
What is Endometriosis?
Your uterus is lined with a special type of tissue known as endometrial tissue that has a unique quality … It grows and sheds every month! This shedding is driven by hormones which are chemical messengers in the body. Estrogen and progesterone are two hormones that play a key role in the building & shedding of your uterine lining.
Why do these hormones cause this cycle? Well, they cause the lining of your uterus to thicken so if a pregnancy occurs, an egg can implant into this thick uterine wall. Think of the uterus as a home! If you want a child to grow safely in this home, you as a mother, would want strong walls, not flimsy ones! However, if a pregnancy does not occur, the body and its hormones do not want to keep these strong walls. Instead, they break down the lining of the uterus and shed it. This is your menstrual cycle or period.
So, let’s think about this cycle with endometriosis now.
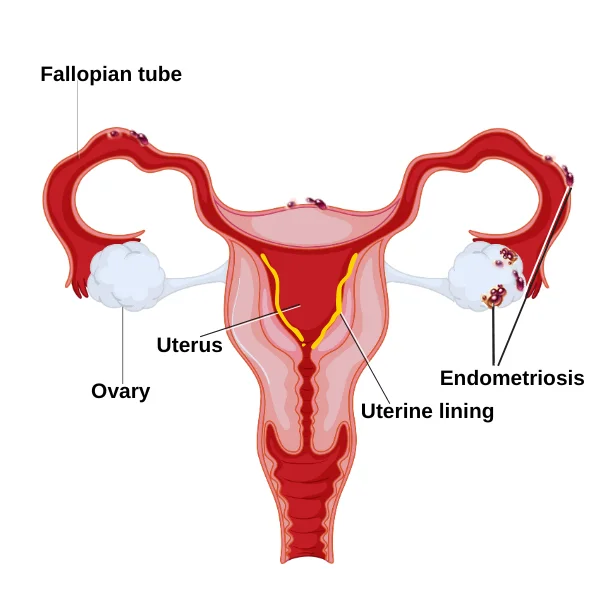
Endometriosis is an inflammatory condition that occurs when the special, endometrial tissue grows outside of the uterus. Remember, that tissue is supposed to stay inside the uterus because that’s where a baby would grow! When the endometrial tissue grows outside, it is in the wrong location, but it’s still endometrial tissue with the same unique quality. That means that it still responds to hormones like estrogen & progesterone and will shed every month. This essentially leads to internal bleeding, inflammation of local tissue, internal scarring, organ damage, and a wide spectrum of health complications, such as fertility issues. As you can see from the image below endometriosis leads to these lesions and scars in many areas of the reproductive tract & other organs as well.
Endometriosis impacts every 1 in 10 women globally, most commonly between 20-35 years of age (2). However, the cause of endometriosis is unknown and there is no current cure, but there are ways to manage it and slow it down. Clearly, this health condition deserves far more attention.
Endometriosis Symptoms: What Does Endometriosis Pain Feel Like?
Endometriosis has several distinguishing symptoms, yet, these signs are also shared with other health conditions. Such similarities cause misdiagnosis of symptoms and contribute to the long time it takes many women to get an endometriosis diagnosis.
The most common sign of endo is intense pain. This pain can be experienced in the abdominal, back, pelvis, and even distant sites like the shoulder blades. Women often experience this pain with intercourse, bowel movements, and urination. Most women are more than familiar with the pain that comes from a normal menstrual cycle, called “period cramps”. Normal period cramps typically begin just before your period, no more than 24 hours before and continue for no more than 3 days. That’s what defines a “normal period pain” window. A notable difference in endometriosis is that this pain can sometimes span longer than normal period pain (3). Are you finding yourself in more pain each month than not? If your pain falls outside of the normal window, check in with your provider. Also, check out our blog, Magnesium for Period Cramps Relief, for using magnesium for endo & period pains.
Women also may experience heavy menstruation, constipation, swollen abdomen, gas, depression, insomnia, and lethargy. That’s why a common misdiagnosis is Irritable Bowel Syndrome (IBS) because it shares the characteristics and symptoms mentioned above. However, IBS is a chronic gastrointestinal disorder while endometriosis is a chronic inflammatory, gynecological condition.
While pain and abdominal discomfort are common factors, there are also situations of “silent endometriosis”. In these cases, endometrial tissue still grows outside of the uterus but the patient has no symptoms and does not experience common signs like pain. As you can imagine, these nonexistent signs result in a delay in diagnosis or no diagnosis at all. Silent endometriosis is usually discovered with unexplained infertility.
Endometriosis: How is it Diagnosed?
Laparoscopy is the best and only reliable method for diagnosing endometriosis. This term is a minor surgical procedure where the doctor will use a small instrument to look for endometrial tissue outside of the uterus. A tissue sample may be taken to confirm the diagnosis.
Though laparoscopy is the only way to confirm an endo diagnosis, other tests, like a physical exam or imaging, can present clues about the condition.
For example, during a physical exam, a professional can feel irregular growth, tenderness, and painful spots in the pelvic area. However, a woman can have a normal examination yet still have endometriosis. Again, this highlights the reasoning behind delays in diagnosis.
An ultrasound and magnetic resonance imaging (MRI) are two noninvasive forms of imaging that can help identify endometriosis. An ultrasound test uses sound waves to create pictures of internal body structures. The MRI exam also produces images of internal organs but uses magnetic fields and radio waves. It can detect deep sites of endometrial tissue and show a bit more detail of the organs. While these two tests cannot definitively confirm endo 100%, they can sometimes confirm suspicions and help us lead us in the right direction. But again, they may come back clear even with endometriosis being there, that’s why laparoscopy is the gold standard for diagnosing endometriosis.
Endometriosis is a Chronic Pain Condition: Why is there Stigma?
As you learned from this blog, endometriosis is a serious, often extremely painful, and common health condition that impacts so many women globally. However, there is a mark of shame or stigma that surrounds endometriosis. Endo might make day-to-day activities incredibly hard because of symptoms like severe abdominal and pelvic pain, GI discomfort, fatigue, infertility, and abnormal menstruation. This can cause major negative impacts on an individual’s physical, mental, and social well-being (4). Many women with the condition are also not taken seriously. Questioning and doubting pain severity by doctors, family, friends, and employers causes relationship strain and feelings of isolation.
The frustration, towering medical bills, and invalidation of this suffering are nearly unimaginable. Do not be afraid to advocate for yourself. You are the only person that truly knows your body and health. If you feel as if you are not being taken seriously by your health provider, then fearlessly find a new one. It certainly can be hard to find a new health provider that is better for you. Perhaps you have seen them for decades, feel comfortable with them, or lack the time to search. However, even the most talented physicians are often unaware of the impact of lifestyle factors on endo. For example, there are several root causes like diet, stress, and sleep that significantly influence endo symptoms. Please read The 6 Root Causes Behind Your Endometriosis Symptoms for more information!

This is an example we often share with our patients and we hope it offers a new perspective when you are considering a switch! When you go to shop for a car, you likely will go to multiple dealerships, research multiple vehicle models, and test drive multiple cars. You do this to find the best brand, model, and price for you! Similarly, when you go to confront a health issue, you should visit several healthcare providers, research several medical specialties, and even “test-drive” several professionals. Again, you do this to discover the best healthcare team and treatment approach to address your condition and symptoms. Remember, your health is far more important than a car, so all the more reason to do a thorough search!
If your medical provider or those in your life have ignored your call for help with endometriosis, we hear you. By confronting the root causes of your symptoms and providing highly specific care for each of our patients, we work hard to help our patients properly advocate for the correct diagnosis & treatment. By providing tools to help advocate for your condition, we also hope to increase early conversations about endometriosis symptoms, so no more women have to suffer alone in silence.
Let’s bring an end to endo stigma!
Now that you know what endo is all about, the next step is to figure out your treatment options.
You can check out our endometriosis page here to see how we help our patients suffering with endometriosis feel in control again.
References
- Frankel LR. A 10-Year Journey to Diagnosis With Endometriosis: An Autobiographical Case Report. Cureus. 2022;14(1):e21329. Published 2022 Jan 17. doi:10.7759/cureus.21329
- Rolla E. Endometriosis: advances and controversies in classification, pathogenesis, diagnosis, and treatment. F1000Res. 2019;8:F1000 Faculty Rev-529. Published 2019 Apr 23. doi:10.12688/f1000research.14817.1
- Normal Menstrual Cramps or Endometriosis: How to Tell the Difference: OB-GYN Associates of Marietta: Obstetrics and Gynecologist. Accessed June 26, 2024. https://www.obgynassociatesmarietta.com/blog/normal-menstrual-cramps-or-endometriosis-how-to-tell-the-difference
- Sims, O. T., Gupta, J., Missmer, S. A., & Aninye, I. O. (2021). Stigma and Endometriosis: A Brief Overview and Recommendations to Improve Psychosocial Well-Being and Diagnostic Delay. International journal of environmental research and public health, 18(15), 8210. https://doi.org/10.3390/ijerph18158210


