Birth control = no pregnancy … Duh! Everyone knows that! But have you ever wondered if that’s all it does? Even though birth control is most known for its use to prevent pregnancy, it has other uses as well. In fact, it is actually one of the most effective forms of medical treatment for endometriosis. You might be thinking: “But how dare you say that???! I thought birth control was bad for you?!” Hear us out. We’re 100% with you that birth control is highly overprescribed and misused. However, there are a few circumstances where the benefits may outweigh the risks.
Hold tight, it’ll all make sense in a bit. Yes, birth control is not always a great option for many gynecologic conditions, but sometimes it is. That nuance is very important. And a good practitioner should never speak in extremes. Every condition and every woman has different needs. So yes our advice will differ a lot depending on the situation. Endometriosis in particular is a good example of this. While birth control cannot cure the condition, it can reduce the growth of endometrial tissue and pain (1). This is particularly important because endometriosis is a condition that comes with many risk factors if it’s uncontrolled.
Before we dive in, let’s remind ourselves of some important processes that are often forgetten but are crucial to endometriosis…hormones and the ovarian cycle.
What is Endometriosis?
A woman’s uterus is lined with endometrial tissue which is very special type of body tissue. It has a unique property – it grows and breaks down every month!
Why? It grows in case a woman becomes pregnant and needs to build a strong home for a baby in the uterus. It breaks down if a woman does not and will exit the body as a “period”.
How? This tissue responds to hormones like estrogen and progesterone.
In the middle of this cycle, estrogen levels rise and your ovaries release an egg, also called ovulation. If pregnancy occurs, this egg will make itself at home within the growing endometrial tissue.
So to recap, estrogen plays two roles: (1) signal ovulation and (2) build a home for a fertilized egg inside of the uterus – which is called endometrial tissue.
Let’s think about this with endometriosis. Endometriosis is a chronic condition where endometrial tissue grows outside of the uterus, even though it should only grow inside.
However, this endometrial tissue still responds to estrogen and estrogen still sends the same signals. Estrogen wants to build a home inside of the uterus, but instead, it is also building outside of the uterus – where an egg would never go! That’s the issue with endometriosis. Just like constructing an actual house in the incorrect location, this is a ton of wasted material and energy. At the end of your cycle if the egg did not fertilize, the body wants to shed the endometrial tissue it build (i.e., it’s time for your period). But, with endo, this endometrial tissue is both inside and outside of the uterus. The endometrial tissue that’s outside the uterus has nowhere to leave the body because the exit for endometrial tissue is through the vagina. With endometrial tissue outside the uterus, the sticky bloody tissue gets stuck between your organs. This causes many issues. If you have read our blog, Do I Have Endo: Endometriosis, Symptoms, and Diagnosis, you know endo causes inflammation of local tissue, internal scarring, organ damage, infertility, and severe pain.
In our last blog, The 6 Root Causes Behind Your Endometriosis Symptoms: What You Need to Know, we explored the ways that diet and nutrition can influence the effects of endometriosis in your life. While foods can alleviate symptoms, medications may sometimes be needed. Specifically, medications in combination with nutrition and herbal strategies can best support those with more severe cases of endometriosis or those who are not experiencing a significant decrease in symptoms. Though adjusting your diet or lifestyle can feel less scary than using medicine, it is important to understand all of your options. In fact, the combination of lifestyle changes with medication can often show the best treatment results!
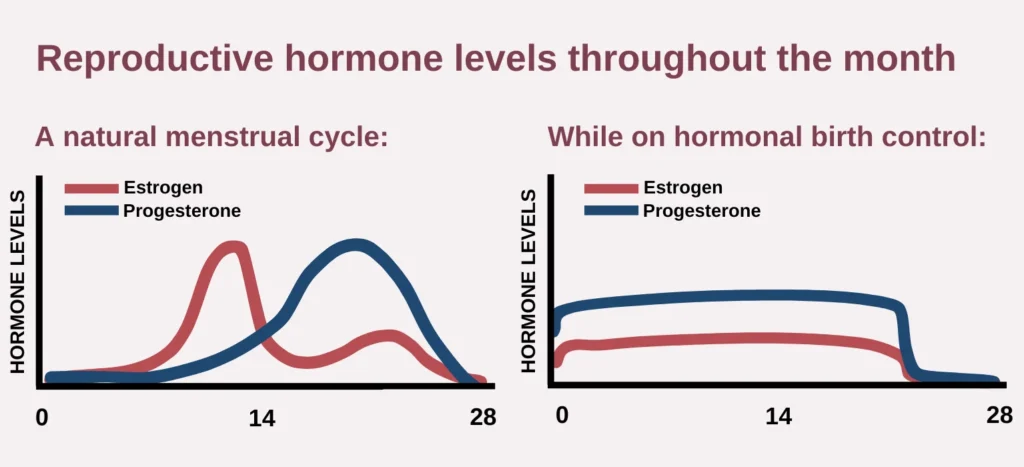
Birth control is a type of hormonal medication that changes the level of specific hormones: estrogen and progesterone. Remember, these hormones are responsible for sending signals during the menstrual cycle like ovulation or the growth of endometrial tissue (1). Remember, estrogen signals endometrial tissue growth and ovulation. Progesterone helps to stabilize the endometrial tissue; it keeps it nice and fluffy for a potential baby.
Normally, estrogen and progesterone levels rise and fall like a rollercoaster to send their signals. Look at the left side of the graph below …
Estrogen levels are very high in the first half of our cycle because it signals endometrial tissue growth and ovulation. Progesterone, however, is only high in the second half of our cycle. These high levels help prepare the uterus for potential pregnancy. When pregnancy does not occur, progesterone levels drop and this results in your period.
Now look at the right side of the graph below…
When using hormonal birth control, both progesterone and estrogen levels remain constant. Since high levels of estrogen lead to more endometrial tissue growth and painful symptoms, we want estrogen to be at a constant lower level. In addition, you can see that birth control gives you more progesterone than estrogen. This is helpful because having more progesterone helps to reduce endometrial tissue growth. Think of estrogen like a construction worker, it just keeps building that endometrial tissue. But progesterone is like a construction truck that stands in its way, telling estrogen “Stop! We don’t need any more building!” Therefore, by having a constant level of progesterone every day and no more estrogen rollercoasters, the body makes less endometrial tissue. This is actually why pregnancy also helps endometriosis. When you’re pregnant progesterone is at its highest, and your body has much less endometrial tissue growth outside the uterus. In essence, more progesterone helps to balance out the effects of estrogen and over time helps to inhibit endometrial tissue growth. Progesterone is also anti-inflammatory so that’s another benefit too! Overall, these changes cause a woman’s period to be shorter, lighter, and less painful (2)! Pretty cool right?
Birth Control for Endometriosis: Which Do I Choose??
There are many types and forms of birth control to choose from. Just like brands of shampoo, it can be very frustrating and overwhelming to figure out which is the best birth control for endometriosis. Each option has its pros and cons. For example, all medications, like birth control, come with side effects and affect each person differently. Endometriosis symptoms on birth control can nearly disappear for one woman but not for another. So, talk to your gynecologist or medical provider to find the best option for you!
- Combined Hormonal Medication – this option is a combination of estrogen and progestin (a form of progesterone). It suppresses the period and helps to stop endo from progressing, which helps to reduce endometriosis pain. These hormones can be delivered in the form of …
- Estrogen-Progesterone combined birth control pills
- Vaginal Ring (estrogen-progesterone combined)
- Patch (estrogen-progesterone combined)
- Progestin-Only Hormonal Medication – this option only contains progestin that mimics the hormone, progesterone. It’s a good option for women who want to avoid estrogen-containing birth control pills. It helps to decrease the effects of estrogen and the growth of endometrial tissue (3). This hormone can be delivered in the form of …
- Progestin-only birth control pills
- For some women, this type of birth control can be weaker or less effective than the estrogen-progesterone combined birth control pills
- Hormonal Intrauterine Devices (IUD) like the Mirena®, Liletta®, Kyleena® and Skyla®
- Many women with endo find a lot of relief with this type of birth control. The progesterone hormone is delivered straight to the uterus and surrounding tissue, potentially making it more effective.
- Progestin-only birth control pills
- Other options – Gonadotrophin-releasing hormone agonists and Danazol are two other options for medications (4). However, they can block hormones completely which significantly increases side effects, and are unsafe long-term. So, we do not prefer or recommend these options as a first choice.
Phew! We covered a ton of information!! We know this is very overwhelming but, don’t forget that it is also exciting! One of these options in combination with nutrition & herbal medicine tools can truly transform your life with endo.
Remember that birth control combined with functional and integrative medicine often leads to the best results. What is functional and integrative medicine? Functional and integrative medicine applies a root-cause and holistic approach to health issues by taking into account all aspects of your lifestyle that are impacting your body. These disciplines often use lifestyle changes in nutrition, stress management, herbal medicine, and more. Read our blog, The 6 Root Causes Behind Your Endometriosis Symptoms: What You Need to Know, to learn about what root causes we tend to look at in endometriosis!
We are super excited to help guide you through endometriosis treatment and answer the countless questions that we know you have! If you’re ready to take that next step in taking control of your endometriosis, head to our services page here.
References
- Nirgianakis K, Egger K, Kalaitzopoulos DR, Lanz S, Bally L, Mueller MD. Effectiveness of Dietary Interventions in the Treatment of Endometriosis: a Systematic Review. Reprod Sci. 2022;29(1):26-42. doi:10.1007/s43032-020-00418-w
- Williams RS. Benefits and risks of oral contraceptive use. Postgrad Med. 1992;92(7):155-157, 161. doi:10.1080/00325481.1992.11701539
- Morotti, M., Remorgida, V., Venturini, P. L., & Ferrero, S. (2014). Progestogen-only contraceptive pill compared with combined oral contraceptive in the treatment of pain symptoms caused by endometriosis in patients with migraine without aura. European Journal of Obstetrics & Gynecology and Reproductive Biology, 179, 63-68. https://doi.org/10.1016/j.ejogrb.2014.05.016
- Magon N. Gonadotropin releasing hormone agonists: Expanding vistas. Indian J Endocrinol Metab. 2011;15(4):261-267. doi:10.4103/2230-8210.85575


